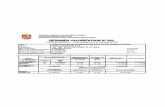
107486_DYSMENORRHOEA
Transcript of 107486_DYSMENORRHOEA
-
8/19/2019 107486_DYSMENORRHOEA
1/15
DYSMENORRHOEA
-
8/19/2019 107486_DYSMENORRHOEA
2/15
Dysmenorrhea
is defined as severe, cramping pain in the
lower abdomen that occurs just before or
during menses.
(primary or secondary)
Primary dysmenorrhoea occurs in the
absence of significant pelvic pathoIogy. usuallydevelops within the first 2 years of the
menarche
-
8/19/2019 107486_DYSMENORRHOEA
3/15
Characteristics of primary dysmenorrhoea
The pain is often intense, cramping, crippling and severelyincapacitating so that it causes a major disruption of socialactivities.
It is usually associated with the onset of menstrual blood loss
but may begin on the day preceding menstruation. The pain only occurs in ovulatory cycles, is lower abdominal in
nature but sometime radiates down the anterior aspect of thethighs.
The pain often disappears or improves after the birth of the first
child. Dysmenorrhoea is often associated with vomiting and diarrhoea Pelvic examination reveals no abnormality of the pelvic organs.
-
8/19/2019 107486_DYSMENORRHOEA
4/15
Pathophysiology of primary dysmenorrhoea
Primary dysmenorrhoea is a feature of ovulatory cycles andusually appears within to !2 months of the menarche.
The etiology of primary dysmenorrhea has been attributed touterine contractions or ischemia, psychological factors, and
cervical factors. Psychological factors may alter the perception of pain but are
not uni"ue to the problem of dysmenorrhea.
There is no convincing evidence of cervical stenosis in patients
with dysmenorrhea, so there is no basis for incriminating cervicalstenosis or psychological factors as major contributors to the
problem of primary dysmenorrhea.
-
8/19/2019 107486_DYSMENORRHOEA
5/15
Pathophysiology of primary dysmenorrhoea
#omen with dysmenorrhea have increased uterine activity, which may manifest as increased resting tone, increasedcontractility, increased fre"uency of contractions, or incoordinateaction.
Prostaglandins are released as a conse"uence of endometrialcell lysis with instability of Iysosomes and release of en$ymes.which brea% down cell membranes
The evidence that prostaglandins are involved in primary
dysmenorrhoea is convincing. &enstrual fluid from women withdysmenorrhea has higher than normal levels of prostaglandins'especially P()2a and P(*2+, and these levels can be reducedto below normal with nonsteroidal antiinflammatory drugs'-/IDs+. which are effective treatments.
-
8/19/2019 107486_DYSMENORRHOEA
6/15
Clinical Symptoms
Primary dysmenorrhoea usually begins to !2months after menarche, almost invariably coincidingwith the onset of ovulatory cycles. Patients complain
of spasmodic or cramping lower abdominal pain thatmay radiate suprapubically or to the inner aspect ofthe thighs. They may have bac%ache of varyingseverity. They may also have other accompanyingsymptoms, such as headache, nausea,vomiting,
diarrhea, or fatigue. ymptoms typically last 01hours or less, but sometimes may last up to 2hours.
-
8/19/2019 107486_DYSMENORRHOEA
7/15
Secondary dysmenorrhoea
Secondary dysmenorrhoea is caused by organic pelvicpathology and it usually has its onset many years after themenarche.
/ny woman who develops secondary dysmenorrhoea should be
considered to have organic pathology in the pelvis until provedotherwise.
Pelvic examination is particularly important in this situation and, ifthe findings are negative, laparoscopy is indicated.
3ommon associated pathologies include endometriosis,
adenomyosis, pelvic infections and intrauterine lesions such as submucous,fibroid.
-
8/19/2019 107486_DYSMENORRHOEA
8/15
Pathophysiology of secondary
dysmenorrhoea
The mechanism of pain in secondarydysmenorrhoea is due to pelvic congestion
which is more mar%ed in the premenstrual
period.
Pain increases in its severity as menstruationapproaches and is relieved by the onset of
menstrual flow, due to the diminution of pelvic
congestion.
-
8/19/2019 107486_DYSMENORRHOEA
9/15
Clinical Symptoms
econdary dysmenorrhoea usually starts fewdays 'about 4 to 5 days+ before menstruation.
Pain is continuous dull aching lower
abdominal pain accompanied by bac%acheoccurring in parous women after many yearsof relatively painless menstruation.
econdary dysmenorrhoea may beassociated with other symptoms asdyspareunia, infertility and abnormalbleeding.
-
8/19/2019 107486_DYSMENORRHOEA
10/15
Management
Primary dysmenorrhoea:General and psychological treatment: Discussion and reassurance are an essential part of
management. Primary dysmenorrhoea tends to presentsome months after the menarche and is associated withovulatory cycles, early cycles frequently beinganovulatory. The intensity of pain may be aggravated byapprehension and fear, and reassurance that the pain does
not indicate any serious disorder may lessen thesymptoms. It is also common for the pain to eitherdisappear or substantially lessen after the birth of the firstchild.
-
8/19/2019 107486_DYSMENORRHOEA
11/15
Drug therapy: Dysmenorrhoea can be effectively treated by drugs
that inhibit prostaglandin synthesis and hence uterine
contractility. These drugs include aspirin, mefenamic acid, naproxen
or ibuprofen. /s dysmenorrhoea is often associated withvomiting, headache and di$$iness, it may be advisable tostart therapy either on the day before the period is
expected, or as soon as the menstrual flow commences &efenamic acid is given in a dose of 256 mg hourly.
This drug also reduces menstrual flow in some womenwith menorrhagia.
-
8/19/2019 107486_DYSMENORRHOEA
12/15
If these drugs are inade"uate, suppression ofovulation with the contraceptive pill is highlyeffective in reducing the severity of dysmenorrhoea.#here it is ineffective, then careful consideration
should be given to the possibility of underlyingpathology.
If all conservative medical therapy fails, then reliefmay sometimes be achieved by mechanicaldilatation of the cervix or by the surgical removal ofthe pain fibers to the uterus in an operation %nownas presacral neurectomy, but these methods oftreatment should be approached with considerablecaution.
-
8/19/2019 107486_DYSMENORRHOEA
13/15
Physical therapy *ncourage regular and aerobic exercises in fresh air
to raise their general health . 7elaxation techni"ues, as well as meditation and
hypnosis may be helpful for raising their pain
threshold. /void constipation. &assage . 8ot pac%s on the lower abdomen for !6!5 minutes. /ccupressure on the lumosacral area and 4 cm
superior to the medial malleolus.
-
8/19/2019 107486_DYSMENORRHOEA
14/15
T*-
9ow level laser therapy
-
8/19/2019 107486_DYSMENORRHOEA
15/15
Secondary dysmenorrhoea:
In cases of secondary dysmenorrhoea, the
treatment is dependent on the nature of theunderlying pathology. If the pathology is not
amenable to medical therapy, the symptoms
may only relieved by hysterectomy. 8owever,
the role of physical therapy in such cases willconsist of pre and post operative physical
treatment.