feocromocitoma
-
Upload
gaby-isela-sifuentes-lucio -
Category
Documents
-
view
216 -
download
2
Transcript of feocromocitoma

REVIEWwww.nature.com/clinicalpractice/endmet
Pheochromocytoma: recommendations for clinical practice from the First International SymposiumKarel Pacak, Graeme Eisenhofer, Håkan Ahlman, Stefan R Bornstein, Anne-Paule Gimenez-Roqueplo, Ashley B Grossman, Noriko Kimura, Massimo Mannelli, Anne Marie McNicol and Arthur S Tischler*
INTRODUCTIONThe 2004 WHO classification of endocrine tumors defines pheochromocytoma as a tumor arising from catecholamine-producing chromaffin cells in the adrenal medulla—an intra-adrenal para-ganglioma. Closely related tumors of extra-adrenal sympathetic and para sympathetic paraganglia are classified as extra-adrenal paragangliomas. Although arbitrary, this nomen clature serves to emphasize the distinctive proper ties of tumors in different locations. In contrast to adrenal and extra-adrenal sympathetic para gangliomas, those from para sympathetic tissue (mainly in the head and neck) rarely produce significant amounts of catecholamines.
Improvements in diagnosis, localization, manage-ment, and treatment of pheo chromocytomas and catecholamine-producing paragangliomas are being driven by recent leaps in understanding of the genetics and biology of these tumors, coupled with advances in analytical chemistry, gen omics, molecular biology, biotechnology, and nuclear medicine. Ineffective treatments for malignant tumors, inadequate methods to distinguish malignant from benign disease, and a lack of consensus on how to apply recent scien-tific and medical advances to improve diagnosis and patient manage ment remain important un resolved problems.
This article reviews progress and outlines recom-mendations for improved clinical evalua tion and care of patients with catecholamine-producing paragangliomas; it is based on presentations and moderated ‘break-out’ discussion sessions at the First International Symposium on Pheochromocytoma (ISP) held on 20–23 October, 2005, at Bethesda, MD, USA. Break-out sessions were designed to foster resolution of outstanding issues and problems in the form of recom-mendations addressing a series of questions (Box 1) formulated by key opinion leaders in the field, with input from patients and their support-group repre-sentatives and final agreement at a general session in which all attendees could be present. Here, we will discuss each of these questions in turn.
SUMMARYThe First International Symposium on Pheochromocytoma, held in October 2005, included discussions about developments concerning these rare catecholamine-producing tumors. Recommendations were made during the symposium for biochemical diagnosis, localization, genetics, and treatment. Measurement of plasma or urinary fractionated metanephrines, the most accurate screening approach, was recommended as the first-line test for diagnosis; reference intervals should favor sensitivity over specificity. Localization studies should only follow reasonable clinical evidence of a tumor. Preoperative pharmacologic blockade of circulatory responses to catecholamines is mandatory. Because approximately a quarter of tumors develop secondary to germ-line mutations in any one of five genes, mutation testing should be considered; however, it is not currently cost effective to test every gene in every patient. Consideration of tumor location, presence of multiple tumors, presence of metastases, and type of catecholamine produced is useful in deciding which genes to test. Inadequate methods to distinguish malignant from benign tumors and a lack of effective treatments for malignancy are important problems requiring further resolution.
KEYWORDS diagnosis, genetics, localization, paraganglioma, pheochromocytoma
K Pacak is a senior investigator at the National Institute of Child Health and Development, NIH, Bethesda, MD, USA. G Eisenhofer is a staff scientist at the NIH. H Ahlman is Professor of Endocrine Surgery at the Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden. SR Bornstein is Professor and Chair of Medicine at the Carl Gustav Carus University Hospital, Department of Medicine, Dresden, Germany. A-P Gimenez-Roqueplo is an Associate Professor in Genetics at the Assistance Publique des Hopitaux de Paris, Hospital Européen Georges Pompidou, Universite Paris Descartes, Paris, France. AB Grossman is Professor of Neuroendocrinology in the Department of Endocrinology at the St Bartholomew’s Hospital, Barts and the London School of Medicine, London, UK. N Kimura is a pathologist and investigator at the Tohoku Rosai Hospital, Sendai, Japan. M Mannelli is a Professor of Endocrinology at the Department of Clinical Pathophysiology, University of Florence, Florence, Italy. AM McNicol is a reader in pathology at the University of Glasgow, Glasgow, UK. AS Tischler is Professor of Pathology at the Tufts University School of Medicine, Boston, MA, USA.
Correspondence*Department of Pathology, Tufts – New England Medical Center, 750 Washington Street, Boston, MA 02111, [email protected]
Received 29 March 2006 Accepted 15 September 2006
www.nature.com/clinicalpracticedoi:10.1038/ncpendmet0396
REVIEW CRITERIAThis article is based on sessions at the International Symposium on Pheochromocytoma 2005 meeting.
92 NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM FEBRUARY 2007 VOL 3 NO 2
NCPEM_2005_152.indd 92NCPEM_2005_152.indd 92 8/1/07 1:42:50 pm8/1/07 1:42:50 pm

REVIEW
FEBRUARY 2007 VOL 3 NO 2 PACAK ET AL. NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM 93
www.nature.com/clinicalpractice/endmet
Considering the absence of large, randomized, double-blind, multicenter clinical trials fulfilling firm, high-level evidence-based criteria, recom-mendations from a consensus of experts from around the world seemed appropriate to provide guidance for the clinical community. During the course of discussions, it became clear that strict guidelines are rendered in appropriate by variability in the presentation of tumors and international differences in medical approaches or the availability of tests and therapies. Recommendations are, therefore, intended to complement sound clinical judgment, and are not intended as rigid mandates.
This article attempts to provide an un biased overview of the consensus recom mendations from the break-out sessions of the ISP. It acknowledges that there are numerous opinions and approaches and is not meant to favor any specific point of view, including those of the authors. Because of the limitations of space and the number of refer-ences, many ramifications of the topics and discus-sions are not dealt with in detail. Comprehensive reviews of the literature related to manage-ment and diagnosis of pheo chromocytoma are available elsewhere.
BIOCHEMICAL DIAGNOSISPheochromocytomas and extra-adrenal para-gangliomas are rare, and often overlooked, causes of hypertension. The crucial first step is there-fore to consider these tumors when thinking of possible diagnoses. Confirming the diagnosis requires biochemical evidence of inappropriate catecholamine production. Measurement of urinary catecholamine levels has traditionally been the most widely used test, but measurement of urinary catecholamine metabolites or plasma catecholamines has also been recommended.1–3
Previous recommendations on preferred biochemical tests—more often based on insti-tutional experience than evidence-based medi-cine—are now being reconsidered in light of technical advances and improved understanding of catecholamine metabolism.4 It is now clear that catecholamines are metabolised within chro-maffin cells to metanephrines (i.e. norepinephrine to normetanephrine and epinephrine to meta-nephrine). This intratumoral process occurs inde-pendently of catecholamine release, which can occur intermittently or at low rates. Consistent with these concepts, studies have confirmed that measurements of fractionated metanephrines (i.e. normetanephrine and metanephrine measured
separately) in urine or plasma provide superior diagnostic sensitivity to measurements of the parent catecholamines.5–11
An important recommendation derived from the above considerations, and endorsed by those at the ISP, was that initial testing for pheo-chromocytoma should include measurements of fractionated metanephrines in urine or plasma, or both, as available. There was no consensus on whether plasma or urine measurements should be the preferred test. Plasma metanephrines are usually measured in their free form, as produced
Box 1 Unresolved issues concerning pheochromocytomas and paragangliomas.
Biochemical diagnosisWhat are the preferred biochemical tests or testing algorithms for confirming or excluding the presence of a tumor and what cost–benefit factors should be considered?
What precautions should be considered to minimize or avoid false-positive results or drug interference during biochemical testing?
Tumor localizationWhat evidence for the presence of a tumor justifies imaging studies?
What imaging strategies are appropriate and how should they be applied?
GeneticsShould all patients with pheochromocytomas or paragangliomas undergo genetic testing for possible disease-causing gene mutations or should this be confined to selected patients?
What cost–benefit factors should be considered in genetic testing?
Patient managementWhich are the most appropriate strategies for management of patients before, during, and after surgery?
Which drugs and doses should be used, and what clinical parameters should be monitored?
Which surgical approaches or alternatives to surgery should be considered for adrenal and extra-adrenal tumors?
What is the appropriate method for follow-up of patients after surgical resection of a tumor?
PathologyCan a reliable scoring system be developed to identify high-risk or poor-prognosis tumors?
Can pathology be helpful in identifying tumors with particular gene mutations?
Which ancillary immunohistochemical studies should be performed for risk assessment and phenotype characterization?
Malignant pheochromocytoma or paragangliomaWhat can be done for patients with malignant tumors?
Is chemotherapy or meta-iodobenzylguanide radionuclide therapy useful, and can these therapies be improved or tailored according to the tumor characteristics?
Which approaches can be used to identify new targets for treatment and develop new drugs for these targets?
NCPEM_2005_152.indd 93NCPEM_2005_152.indd 93 8/1/07 1:42:53 pm8/1/07 1:42:53 pm

REVIEW
94 NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM PACAK ET AL. FEBRUARY 2007 VOL 3 NO 2
www.nature.com/clinicalpractice/endmet
by tumors, whereas urinary metanephrines are commonly measured after a deconjugation step and largely represent sulfate-conjugates produced by an enzyme localized mainly to gastrointestinal tissues. This might explain the diagnostic advantages of plasma measurement compared with urinary measurement reported by two groups.8,11 The reported differences are, nevertheless, relatively small compared with the advantages of either test to tests for the parent catecholamines. Other factors, as outlined in Box 2, might be more important to consider in the choice of plasma or urinary measurements of fractionated metanephrines.
Two further related recommendations arose from the discussion session on biochemical diagnosis: first, reference intervals for plasma and urinary metanephrines should primarily ensure optimum diagnostic sensitivity, with specificity a secondary consideration—this is mainly to avoid the deadly consequences of a missed diagnosis;
and second, testing algorithms should not simply rely on a binary approach for test interpreta-tion (i.e. a result being positive or negative), but should take advantage of the continuous nature of biochemical test results.
The latter recommendation is based on recog-nition that high diagnostic sensitivity is invariably associated with a trade-off in specificity, making it troublesome to distinguish true-positive from false-positive results. Clinical decision-making should, therefore, take into account the extent of the elevation in biochemical test results (Figure 1). Although an elevation of plasma or urinary normetanephrine slightly above the respective upper reference interval might only marginally increase the post-test probability of pheo chromocytoma, an elevation of more than fourfold above the reference interval is associated with a close to 100% probability of the presence of the tumor.12 The actual level of the abnormal result should, therefore, be used to determine the need for immediate tumor localization studies versus additional biochemical investigations.
If there is difficulty in distinguishing false-positive from true-positive results, it was gener-ally agreed by the panel of experts that further biochemical testing is warranted before proceeding to localization studies. There was, however, no specific recommendation on what form this should take, although it was agreed that causes of false-positive results owing to medications and other factors should be considered. For testing involving measurements of plasma meta nephrines, a seated posture during sampling was identified as a factor likely to increase the occurrence of false-positive results for that test. It was, therefore, recommended that blood samples should ideally be collected from patients in the supine position or repeated with sampling in the supine position if initial sampling in the seated position returns positive results in the ‘gray area’.
TUMOR LOCALIZATIONThe panel of experts at the ISP felt strongly that localization of pheochromocytoma or para-ganglioma should only be initiated if the clinical evidence for the presence of tumor is reasonably compelling. If suspicion is derived from signs and symptoms of catecholamine excess, biochemical test results should be strongly positive. If the pretest probability of a tumor is higher, such as in patients with a hereditary predisposition or previous history of the tumor, less compelling biochemical evidence might justify imaging studies.
Box 2 Considerations affecting the choice of urinary fractionated metanephrines versus plasma free metanephrines for diagnosis of pheochromocytoma and paraganglioma.
Urinary fractionated metanephrines Plasma free metanephrines
Measurement is usually carried out after a deconjugation step and, therefore, largely reflects conjugated, rather than free, metabolites
Measurements reflect the free metabolites produced within pheochromocytoma tumor cells
Well-established, widely available test Relatively new test, with increasing availability
Urinary concentrations (200–2,000 nmol/l) make analysis relatively easy
Plasma concentrations (0.1–0.5 nmol/l) can make analysis difficult
Easy for medical staff to implement, with minimal expenditure of time and effort
Blood collections require time and effort by medical staff
24-hour collections can be inconvenient for patients
Blood sampling is relatively more convenient for patients
Potential problems with the reliability of incomplete timed urine collections
Collection and handling of blood samples can be carried out reliably
Difficult to control for influences of daily life on sympathoadrenal function or diet
Influences of diet and sympathoadrenal function are more easily controlled for
In children, 24-hour collections are difficult with results difficult to interpret without age-appropriate reference intervals
In children, blood sampling can be stressful, but results are more easily interpreted without age-appropriate reference intervals
The test is not useful in patients with renal failure
The test can be used in patients with renal failure
NCPEM_2005_152.indd 94NCPEM_2005_152.indd 94 8/1/07 1:42:54 pm8/1/07 1:42:54 pm

REVIEW
FEBRUARY 2007 VOL 3 NO 2 PACAK ET AL. NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM 95
www.nature.com/clinicalpractice/endmet
Several other considerations also impact on localization studies. First, because of peri-odic surveillance of patients with a heredi tary pre disposition to catecholamine-producing tumors—including recently discovered disease-causing genes (see below)—there are further requirements to localize tumors of extremely small size or at unusual locations. Second, because of widespread use of anatomic imaging studies, adrenal incidentalomas have become an important clinical entity for which pheo-chromocytoma must be considered, regardless of signs and symptoms. Third, knowledge of the relationship between adrenal and extra-adrenal tumor locations according to genotype or biochemical phenotype calls for selection of appropriate imaging studies that result in decreased costs, radiation exposure, and the time required for tumor localization.
Except for children, pregnant women, and, rarely, patients with an allergy to contrast
medium, there was no consensus on whether CT or MRI is preferred for initial localization of a tumor. This largely depends on the institutional preference and local expertise. Regardless of whether CT or MRI is used, there was a general agreement that imaging studies should initially focus on the abdomen and pelvis. If a tumor is not found, chest and neck images should be obtained, but with recognition that metastatic lesions in long bones can be missed.
Although CT and MRI have excellent sensitivity for detecting most catecholamine-producing tumors, these anatomic imaging approaches lack the specificity required to unequivocally identify a mass as a pheochromocytoma or paraganglioma. The higher specificity of func-tional imaging—the test of choice is currently 123I-labeled meta-iodobenzylguanide (MIBG) scintigraphy—offers an approach to overcome the limitations of anatomic imaging.13,14 The panel of experts agreed that functional imaging
1,000100101.00.1
0.01
0.1
1.0
10
100
0.31
0.61 2.19
1.20
Increasingprobabilityof a tumor
Increasingprobabilityof a tumor
Plasma normetanephrine concentration (nmol/l)
Pla
sma
met
anep
hrin
e co
ncen
trat
ion
(nm
ol/l)
1,000100101.00.10.01
0.1
1.0
10
100
1,000
1.7
0.7
Urinary normetanephrine concentration (µmol/day)U
rinar
y m
etan
ephr
ine
conc
entr
atio
n (µ
mol
/day
)
Increasingprobabilityof a tumor
Increasingprobabilityof a tumor
10.2
22.3
A B
Figure 1 Scatterplots showing the distributions for plasma concentrations (A) or urinary outputs (B) of normetanephrine versus metanephrine in patients with confirmed pheochromocytoma or paraganglioma (gray squares) compared with patients in whom tumors were excluded (gray dots). The vertical and horizontal dashed lines, respectively, illustrate the upper reference limits for plasma concentrations of normetanephrine and metanephrine (0.61 nmol/l and 0.31 nmol/l) (A) and urinary outputs of normetanephrine and metanephrine (1.7 μmol/day and 0.7 μmol/day) (B) used to determine whether the results are negative or positive (a binary approach to test interpretation). With some exceptions, a tumor can be excluded if both normetanephrine and metanephrine concentrations fall below the upper limits. Exceptions include patients with tumors that produce only dopamine—for whom diagnosis might be based on isolated elevation of methoxytyramine (a metabolite of dopamine)—or patients with very small or microscopic tumors (<1 cm diameter) and no other biochemical evidence or signs or symptoms of catecholamine excess. The gray areas beyond the upper limits indicate areas in which positive results are of insufficient magnitude to enable false-positive and true-positive results to be reliably distinguished, but for which the probability of a tumor increases with increasing magnitude of the result (a continuous approach to test interpretation). Beyond the boundary of gray areas the probability of a tumor approaches 100%.
NCPEM_2005_152.indd 95NCPEM_2005_152.indd 95 8/1/07 1:42:54 pm8/1/07 1:42:54 pm

REVIEW
96 NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM PACAK ET AL. FEBRUARY 2007 VOL 3 NO 2
www.nature.com/clinicalpractice/endmet
is useful. Differences in opinion were, however, expressed regarding whether functional imaging should be used for all tumors and in what sequence the modality should be used in relation to anatomic imaging.
Two main reasons warrant the use of func-tional imaging: first, the modality provides a method to more correctly distinguish pheo-chromocytomas or paragangliomas from other lesions; and second, it enables determination of the extent of disease, including the presence of multiple tumors or metastases. Exceptions for which functional imaging might not be required include adrenal tumors of <5 cm in diameter that are associated with a significant elevation of plasma or urine metanephrine levels. This is because such small tumors rarely meta stasise and epinephrine-producing tumors are almost always located in the adrenal gland.15 If diag-nostic doubt remains after all of the conven-tional imaging studies have been performed, venous catheter studies looking for ‘hot spots’ of catecholamines or metanephrines can occasion-ally be helpful, in addition to an examination of the ratio of epinephrine to norepinephrine in the adrenal veins.
Despite the advantages of 123I-labeled MIBG scintigraphy, its sensitivity is less than optimal, especially for detection of metastases. The use of other functional imaging modalities is, therefore, occasionally necessary. PET imaging using 6-[18F]-fluorodopamine, [18F]-dihydroxy-phenylalanine, [11C]-hydroxyephedrine, or [11C]-epinephrine are very promising, new, specific radionuclide localization techniques for pheochromocytoma.16–21 Several recent studies have demonstrated superiority of these techniques to 123I-labeled or 131I-labeled MIBG scinti graphy.17 Octreoscan and [18F]-fluorodeoxyglucose PET are other imaging options.14,22 These studies are not recommended for initial localization, but should be reserved for patients with negative 123I-labeled MIBG scintigraphy or rapidly growing tumors that have a high metabolic rate or express somato statin receptors.23,24
GENETICSHereditary catecholamine-producing pheo-chromocytomas and paragangliomas can be caused by germ-line mutations in any one of five genes identified to date: the rearranged during transfection (RET) proto-oncogene, in which mutations lead to multiple endocrine neoplasia
type 2 (MEN2); the von Hippel–Lindau (VHL) gene, in which mutations lead to VHL syndrome; the neurofibromatosis type I (NF1) gene, which is associated with von Recklinghausen’s disease; and genes encoding succinate dehydrogenase subunits D (SDHD) and B (SDHB), which are associated with familial nonsyndromic pheo-chromocytomas or paragangliomas.25–36 Mutation in a sixth gene encoding succinate dehydrogenase subunit C, SDHC, have so far been reported only in parasympathetic paragangliomas.
Mutation testing, now routinely available for four of the above genes (RET, VHL, SDHB, and SDHD), demonstrates that germ-line muta-tions are responsible for well in excess of the 10% of tumors previously thought to be heredi-tary.15,37–39 Most importantly, 7.5–27.0% of tumors without an obvious syndrome or family history result from otherwise unsuspected germ-line mutations in one of these four genes (Table 1).29,31,36,40,41 The overall hereditary predisposition for pheochromocytoma is, there-fore, estimated to be approximately 20–30%. The high prevalence of unsuspected mutations indicates a need for more widespread genetic testing of patients with these tumors than is currently practiced.
The panel of experts at the ISP agreed that, although there is now a reasonable argument for more widespread genetic testing, it is neither appropriate nor currently cost-effective to test for every disease-causing gene in every patient with a pheochromocytoma or paraganglioma. Rather, it was stressed that the decision to test, and which genes to test, requires judicious consideration of numerous factors, several of which are noted in Figure 2.
The panel underlined the importance of a complete clinical work-up and specialized genetic consultation to collect family history, outline potential repercussions of genetic testing, and obtain appropriate informed consent. A detailed medical and family history can be particularly important in pointing to an under-lying hereditary condition. In the absence of any family history of pheochromocytoma or para-ganglioma, descriptions of sudden death owing to incompletely explained cardiovascular events in family members could suggest an increased probability of hereditary disease, particularly because it is currently considered that at least 50% of catecholamine-producing tumors remain undiagnosed until death. Clinical manifestations in the patient or other family members might
NCPEM_2005_152.indd 96NCPEM_2005_152.indd 96 8/1/07 1:42:55 pm8/1/07 1:42:55 pm

REVIEW
FEBRUARY 2007 VOL 3 NO 2 PACAK ET AL. NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM 97
www.nature.com/clinicalpractice/endmet
also signal a particular disease-causing gene (e.g. a VHL gene mutation suggested by findings of subtle retinal vascular lesions).
Because hereditary tumors usually occur at a younger age than sporadic tumors, age at presenta-tion is an important factor to consider when deciding to test for disease-causing genes.31,32 Findings that at least 36% of pheochromocytomas or paragangliomas in children occur secondary to germ-line mutations underscore the potential importance of genetic testing in pediatric patients with these tumors.42 Young adults with apparently sporadic tumors are likely to harbor occult germ-line mutations more often than elderly patients with these tumors; however, advanced age at presentation does not preclude familial disease, as evident from the case of a 73-year-old woman with an apparently sporadic pheochromocytoma who was serendipitously tested and found to have MEN2A, leading to the discovery of medullary thyroid carcinoma in a relative.43
Except for the obvious clinical manifesta-tions that can indicate a specific hereditary syndrome (e.g. medullary thyroid cancer in patients with MEN2), the panel of experts recommended that the decision to test for a particular gene might benefit from considera-tion of tumor location, presence of metastases, and type of catecholamine produced by the tumor. Although mutations of the SDHB and SDHD genes are occasionally associated with solitary adrenal tumors, patients with these mutations most commonly present with extra-adrenal para gangliomas, often with multifocal disease.28,29,39–41,44 Testing for SDHD and SDHB gene mutations in patients with extra-adrenal tumors can, therefore, be particularly revealing; furthermore, because SDHB gene mutations
carry a high risk of malignant disease, testing for such mutations in patients with metastases, espe-cially related to extra-adrenal paragangliomas, is particularly warranted (Figure 2).29,40,41
By contrast, malignant disease and extra-adrenal tumors are rare in MEN2, so testing for RET gene mutations is unlikely to be rewarding in these situations; furthermore, because pheo-chromocytomas in patients with MEN2 always produce epinephrine, it is inappropriate to test for RET gene mutations in tumors character ized by an increase in urinary or plasma normeta-nephrine but not metanephrine.45 This differs from pheochromocytomas in VHL syndrome, which do not produce significant amounts of epinephrine, indicating that testing for VHL mutations is inappropriate for tumors character-ized by an increase in plasma or urinary metanephrine, with or without an increase in normetanephrine.45
PATIENT MANAGEMENTThe correct clinical management of patients with pheochromocytoma relies on a close collabora-tion between different specialists.38,46–49 In most patients, the tumor is cured by surgery. Exposure to high levels of circulating catecholamines during surgery could cause hypertensive crises and arrhythmias, which can occur even if patients are preoperatively normotensive and asympto-matic. It was, therefore, recommended that all patients with a biochemically positive pheo-chromocytoma or paraganglioma should receive appropriate preoperative medical management to block the effects of released catecholamines.
Because of wide-ranging practices and inter-national differences in available or approved therapies, and without evidence-based studies
Table 1 Relative frequency of genetic mutations in nonfamilial pheochromocytoma and paraganglioma from different European groups presented during the First International Symposium on Pheochromocytoma, which was held on 20–23 October, 2005, at Bethesda, MD, USA.
Gene Country and reference
Germany and Poland39
(%)
Holland (WNM Dinjens, personal communication) (%)
France40
(%)Spain (M Robledo, personal communication) (%)
VHL 11 4.4 3.5 6
SDHB 4 1.5 7 10
SDHD 4 1.6 0.8 10
RET 5 0 0.4 1
Abbreviations: RET, rearranged during transfection; SDHB, succinate dehydrogenase subunit B gene; SDHD, succinate dehydrogenase subunit D gene; VHL, von Hippel–Lindau gene.
NCPEM_2005_152.indd 97NCPEM_2005_152.indd 97 8/1/07 1:42:55 pm8/1/07 1:42:55 pm

REVIEW
98 NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM PACAK ET AL. FEBRUARY 2007 VOL 3 NO 2
www.nature.com/clinicalpractice/endmet
comparing different therapies, there was no specific recommendation on the preferred drugs for preoperative blockade; α-adrenoceptor antagonists,46,47,49 calcium-channel blockers, or angiotensin-receptor blockers have all been recommended and appear useful.50 For tachy-arrhythmias, β-adrenoceptor or calcium-channel blockers were recommended.46 It was empha-sised that if β-adrenoceptor blockers are used, they should be used only after adequate pretreat-ment with α-adrenoceptor antagonists. Volume expansion was also recommended before and after surgery.
It was recommended that only experienced surgeons perform the surgery, and that the approach take into account the type, site, size, and hereditary background of the tumor.51 The use of laparoscopy as the surgical method of choice for most abdominal pheochromocytomas or paragangliomas is recommended for primary or multiple smaller tumors.52 Currently, tumors up to approximately 10 cm can be removed by
laparo scopy. An adrenal-cortex-sparing proce-dure to prevent permanent glucocorticoid deficiency can be an important consideration in hereditary cases in which bilateral disease is probable. The choice of cortex-sparing surgery should be balanced by the consideration that this will increase the risk of tumor recurrence.53–56
There was general agreement that biochemical testing should be repeated approximately 14 days following surgery to check for remaining disease. Importantly, normal postoperative bio chemical test results do not exclude remaining micro-scopic disease, so patients should not be mis informed that they are cured and no further follow-up is necessary. As outlined by patient representatives at the ISP, the lack of recom-mendations on follow-up seems to remain a significant problem. Although follow-up is especially important for patients identified with mutations in disease-causing genes, there is currently no method of follow-up on the basis of pathologic examination of a resected tumor that can rule out the potential for malignancy or recurrence. Long-term periodic follow-up, therefore, remains recommended for all cases of pheo chromocytoma or paraganglioma.
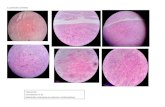
PATHOLOGYPathologic examination should distinguish primary or metastatic pheochromocytomas and para gangliomas from other endocrine or nonendocrine tumors and flag tumors with features suggestive of malignancy or hereditary disease. The latter might include multicentricity, accompanying adrenal medullary hyperplasia, or morphologic findings reported in association with VHL syndrome;57 however, these are not always present.
To be optimally informative, pathology reports must use consistent definitions and incorporate standard elements. The 2004 WHO criteria58 define malignancy by the presence of meta stases, not local invasion. Even extensive invasion—although potentially lethal—is a poor predictor of metastases, and a lack of apparent invasion does not preclude the development of meta stases. The two types of aggressive behavior might, therefore, have different biological under pinnings, requiring different treatment, and should be clearly distinguished in pathology reports.
No histologic feature can—by itself—iden-tify metastatic potential, including capsular or vascular invasion, cytologic atypia, or areas resembling pediatric neuroblastoma; however,
Figure 2 Algorithm for genetic testing for genes associated with pheochromocytoma. The algorithm should be applied if there is a family history of pheochromocytoma, the patient is <50 years old, or there are multiple, malignant, or bilateral tumors. The biochemical phenotype of a tumor should also be considered in selection of the most appropriate genes to test. The term ‘multiple’ in the figure indicates tumors in separate anatomic locations. Patients with multiple endocrine neoplasia type 2 might have multiple tumors in a single adrenal gland. It should be considered that multiple or bilateral tumors often do not occur simultaneously. Abbreviations: RET, rearranged during transfection; SDHB, succinate dehydrogenase subunit B gene; SDHD, succinate dehydrogenase subunit D gene; VHL, von Hippel–Lindau gene.
Informed consent
Differential monitoringGenetic counseling for first-degree family members
Family history or<50 years old
VHLRET
SDHBSDHD
SDHBSDHDVHL
SDHBVHL
RETVHL
SDHD
Multiple Malignant Bilateral
NCPEM_2005_152.indd 98NCPEM_2005_152.indd 98 8/1/07 1:42:56 pm8/1/07 1:42:56 pm

REVIEW
FEBRUARY 2007 VOL 3 NO 2 PACAK ET AL. NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM 99
www.nature.com/clinicalpractice/endmet
some evidence suggests that multifactorial analyses can help to identify tumors with a significant risk of metastasis. Several scoring systems derived from invasion, histologic growth patterns, cytologic features, mitotic activity, and other character istics have been proposed.59–61 One system reportedly predicts both metastatic potential and the clinical course of patients who develop metastases.59 A seminal study by Linnoila et al.60 showed that >70% of sympathoadrenal paragangliomas could be classified correctly on the basis of four factors: extra-adrenal loca-tion, coarse nodularity, confluent necrosis, and absence of hyaline globules. Unfortunately, a number of subsequent papers addressing the assessment of malignancy blur the distinction between intra-adrenal and extra-adrenal tumors, so the powerful independent predictive value of the anatomic site is obscured. Large tumor size (>5 cm) shows some correlation to metastatic potential in some studies, although possibly not as an independently useful criterion.15,59–61
There is currently no consensus on adop-tion of a formal scoring system; however, it is recommended that pathology reports conform to templates or checklists for minimal standard reporting that are endorsed by several pathology associations. The templates list the major elements of the proposed scoring systems and permit addi-tional optional elements. The listing of potentially unfavorable findings will presumably flag a tumor for some type of follow-up, but the nature of the required follow-up remains unclear.
The Association of Directors of Anatomic and Surgical Pathology (ADASP) oversees standard-ization of pathology reporting in the US. ADASP recommendations for reporting of major tumor types are available in pathology journals, in text-books,62 and on the organization’s website.63 The protocols, including those for adrenal gland64 and extra-adrenal paragangliomas,62 were recently updated to generate checklists compliant with the 2004 requirements for accreditation of cancer centers in the US by the American College of Surgery Commission on Cancer. In the UK, the Royal College of Pathologists has recently finalized a more detailed synoptic reporting template,65 based, primarily, on the report by Linnoila et al.60
Pathology practice currently rests mostly on the interpretation of conventional histologic sections stained with hematoxylin and eosin, with ancillary application of immunohistochemistry principally as required for differential diagnosis.
Immunohistochemistry has been used as an ancillary technique for assessment of malignant potential, with mixed results.66 Staining for the proliferation marker Ki-67, which is demon-strated in paraffin sections using the monoclonal antibody MIB-1, is most consistently correlated to malignancy59,67 and is incorporated into the most recently proposed scoring system;59 however, studies of MIB-1 labeling lack methodological consistency and many papers do not provide sufficient methodological detail to permit repli-cation. The Ki-67 labeling index might provide useful information as an optional component of the pathology report, but at present it must be interpreted in the context of individual pathologists’ methods and experience.
MALIGNANT PHEOCHROMOCYTOMAThe incidence of metastatic pheochromocytoma ranges (depending on the genetic background and tumor localization) from 3% to 36%.15,68–71 The survival rate depends on the location of metastatic lesions. Short-term survivors (<5 years) tend to be patients with metastatic lesions in the liver and lungs, whereas long-term survivors are those with metastatic lesions in bones. The overall 5-year survival rate varies between 34% and 60%.69,72 This poor prognosis emphasises the need to adequately identify either those with already existing metastatic disease or, preferably, those who might develop metastases. The latter depends largely on the future discovery of genes and their products that determine meta-static potential and organ specificity. Currently, except for the presence of the SDHB gene muta-tion, there are no reliable markers to suggest a high probability of the development of meta-static pheochromocytoma if a primary tumor is found. Leads from proteomic and genomic studies offer promise for future development of prognostic biomarkers.66,73
Although several therapeutic options exist for patients with metastatic pheo chromocytoma, all options are limited and there is no cure. Reduction of tumor size palliates symptoms, but a survival advantage of debulking is unproven. A reduced tumor burden can facilitate subsequent radio-therapy or chemotherapy. External-beam irra-diation of bone metastases and radio frequency ablation of lesions are treatment alternatives. Chemotherapy with a combination of cyclo-phosphamide, vincristin, and dacarbazine can provide tumor regression and symptom relief in up to 50% of patients, but the responses are
NCPEM_2005_152.indd 99NCPEM_2005_152.indd 99 8/1/07 1:42:57 pm8/1/07 1:42:57 pm

REVIEW
100 NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM PACAK ET AL. FEBRUARY 2007 VOL 3 NO 2
www.nature.com/clinicalpractice/endmet
usually short-lived.74–77 To date, 131I-labeled MIBG therapy is the single most valuable adjunct to surgical treatment of malignant pheo-chromocytomas.78 As a single agent, 131I-labeled MIBG has a limited efficacy of cure, and there is no consensus on what doses to use for treating either bone or organ metastases. Multicenter studies are required to reach a consensus on the efficacy of high-dose versus fractionated medium doses of 131I-labeled MIBG and mono-therapy versus combination therapy with other radio nuclides or modes of chemotherapy.79
CONCLUSIONIt is, generally, agreed that converging techno-logic advances will continue to radically affect the management of patients with pheo chromocytoma or paraganglioma. To be optimally useful and cost-effective, new technologies will need to be thoughtfully integrated with one another and older diagnostic and therapeutic modalities. New biochemical testing methods, involving mass spectrometry, are becoming available at many centers.80–83 Future test reporting should also be improved, to indicate changes in pretest to post-test probabilities of disease for individual patients, to further guide clinical decision-making. For diagnostic imaging, it is probable that combining PET with CT will provide the definitive tool in the near future. The combined methods will increase the accuracy of tumor localization, provide proof that a tumor is, indeed, a pheochromocytoma or paraganglioma, and be useful in monitoring the response to treatment.
Currently, there is no cure for malignant pheo-chromocytoma or paraganglioma and no reli-able histopathologic markers exist to diagnose malignancy or assess prognosis. Establishing the pathways of tumorigenesis and malignancy is an important objective that will be facilitated by advances in understanding the function and genetic basis of these tumors and the wealth of information available on normal chromaffin cell biology; however, histopathology is a time-tested and relatively inexpensive diagnostic tool. Pathology scoring systems reported to correlate to the metastatic potential of tumors and patients’ clinical courses in retrospec-tive studies should be prospectively validated and strengthened by judicious introduction of new immuno histochemical and molecular markers. The future role of pathology, perhaps in combination with genetic testing,66,67 might involve more definitive assessment of
malignancy, genotype–phenotype correlation, and identification of targets for therapy.
Gene expression and proteomic profiling will facilitate the search for new diagnostic and prognostic markers and will present new targets for the treatment of malignancy. Superarrays, using limited numbers of disease-specific genes, could help to quickly and accurately diagnose a tumor and assess its behavior and prognosis. Genes that are as yet unidentified will probably be found to cause hereditary pheochromocytoma or para ganglioma and increase the proportion of hereditary cases above that which has been already estimated. Finally, new animal models of familial and metastatic pheochromocytoma or para-ganglioma will provide essential tools to test new approaches for diagnosis and treatment of tumors and the eradication of tumor precursors.
KEY POINTS■ A pheochromocytoma is an intra-adrenal
paraganglioma; the current WHO nomenclature reserves the term ‘pheochromocytoma’ for paragangliomas of adrenal origin
■ Measurements of plasma or urinary fractionated metanephrines are the most accurate screening procedures
■ Localization studies should only follow reasonable clinical and/or biochemical evidence of a tumor
■ Although CT and MRI have excellent sensitivity for detecting most catecholamine-producing tumors, these anatomic imaging approaches lack the specificity required to unequivocally identify a mass as a pheochromocytoma or paraganglioma
■ Functional imaging offers an approach to overcome the limitations of anatomic imaging—the test of choice currently is 123
I-labeled meta-iodobenzylguanide scintigraphy
■ Laparoscopic surgery is the treatment of choice. Preoperative pharmacologic blockade of adrenergic receptors is mandatory
■ Genetic testing is not currently cost-effective for every gene in every patient; consideration of tumor location, presence of multiple tumors or metastases, and type of catecholamine produced could be useful in deciding which genes to test
■ Malignancy cannot currently be diagnosed by assessment of the primary tumor tissue and is defined by the presence of metastases
NCPEM_2005_152.indd 100NCPEM_2005_152.indd 100 8/1/07 1:42:57 pm8/1/07 1:42:57 pm

REVIEW
FEBRUARY 2007 VOL 3 NO 2 PACAK ET AL. NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM 101
www.nature.com/clinicalpractice/endmet
References1 Bravo EL et al. (1979) Circulating and urinary
catecholamines in pheochromocytoma. Diagnostic and pathophysiologic implications. N Engl J Med 301: 682–686
2 Rosano TG et al. (1991) Advances in catecholamine and metabolite measurements for diagnosis of pheochromocytoma. Clin Chem 37: 1854–1867
3 Young WF Jr (1997) Pheochromocytoma: issues in diagnosis & treatment. Compr Ther 23: 319–326
4 Eisenhofer G et al. (2003) Pheochromocytoma: rediscovery as a catecholamine-metabolizing tumor. Endocr Pathol 14: 193–212
5 Gardet V et al. (2001) Lessons from an unpleasant surprise: a biochemical strategy for the diagnosis of pheochromocytoma. J Hypertens 19: 1029–1035
6 Gerlo E and Sevens C (1994) Urinary and plasma catecholamines and urinary catecholamine metabolites in pheochromocytoma: diagnostic value in 19 cases. Clin Chem 40: 250–256
7 Guller U et al. (2006) Detecting pheochromocytoma: defining the most sensitive test. Ann Surg 243: 102–107
8 Lenders JW et al. (2002) Biochemical diagnosis of pheochromocytoma: which test is best? JAMA 287: 1427–1434
9 Raber W et al. (2000) Diagnostic efficacy of unconjugated plasma metanephrines for the detection of pheochromocytoma. Arch Intern Med 160: 2957–2963
10 Sawka AM et al. (2003) A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and catecholamines. J Clin Endocrinol Metab 88: 553–558
11 Unger N et al. (2006) Diagnostic value of various biochemical parameters for the diagnosis of pheochromocytoma in patients with adrenal mass. Eur J Endocrinol 154: 409–417
12 Eisenhofer G et al. (2003) Biochemical diagnosis of pheochromocytoma: how to distinguish true- from false-positive test results. J Clin Endocrinol Metab 88: 2656–2666
13 Furuta N et al. (1999) Diagnosis of pheochromocytoma using [123I]- compared with [131I]-metaiodobenzylguanidine scintigraphy. Int J Urol 6: 119–124
14 van der Harst E et al. (2001) [(123)I]metaiodobenzyl-guanidine and [(111)In]octreotide uptake in benign and malignant pheochromocytomas. J Clin Endocrinol Metab 86: 685–693
15 O’Riordain DS et al. (1996) Clinical spectrum and outcome of functional extraadrenal paraganglioma. World J Surg 20: 916–921
16 Hoegerle S et al. (2002) Pheochromocytomas: detection with 18F DOPA whole body PET—initial results. Radiology 222: 507–512
17 Ilias I et al. (2002) 6-[18F]-fluorodopamine positron emission tomography versus [131I]-metaiodobenzylguanidine scintigraphy in the evaluation of patients with pheochromocytoma. Abstract P3-511. Presented at the 84th Annual Meeting of the Endocrine Society: 2002 June 19–22; San Fransisco, CA
18 Mann GN et al. (2006) [(11)C]metahydroxyephedrine and [(18)f]fluorodeoxyglucose positron emission tomography improve clinical decision making in suspected pheochromocytoma. Ann Surg Oncol 13: 187–197
19 Pacak K et al. (2001) 6-[18F]fluorodopamine positron emission tomographic (PET) scanning for diagnostic localization of pheochromocytoma. Hypertension 38: 6–8
20 Shulkin B et al. (1992) PET scanning with hydroxyephedrine: A new approach to the localization of pheochromocytoma. J Nucl Med 33: 1125–1131
21 Trampal C et al. (2004) Pheochromocytomas: detection with 11C hydroxyephedrine PET. Radiology 230: 423–428
22 Shulkin BL et al. (1999) Pheochromocytomas: Imaging with 2-[Fluorine-18]fluoro-2-deoxy-D-glucose PET. Nucl Med 212: 35–41
23 Ilias I and Pacak K (2004) Current approaches and recommended algorithm for the diagnostic localization of pheochromocytoma. J Clin Endocrinol Metab 89: 479–491
24 Mamede M et al. (2006) Discordant localization of 2-[18F]-fluoro-2-deoxy-D-glucose in 6-[18F]-fluorodopamine- and [123I]-metaiodobenzylguanidine-negative metastatic pheochromocytoma sites. Nucl Med Commun 27: 31–36
25 Astuti D et al. (2001) Germline SDHD mutation in familial phaeochromocytoma. Lancet 357: 1181–1182
26 Astuti D et al. (2001) Gene mutations in the succinate dehydrogenase subunit SDHB cause susceptibility to familial pheochromocytoma and to familial paraganglioma. Am J Hum Genet 69: 49–54
27 Baysal BE et al. (2000) Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science 287: 848–851
28 Baysal BE et al. (2002) Prevalence of SDHB, SDHC, and SDHD germline mutations in clinic patients with head and neck paragangliomas. J Med Genet 39: 178–183
29 Gimenez-Roqueplo AP et al. (2003) Mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res 63: 5615–5621
30 Maher ER et al. (1991) Von Hippel-Lindau disease: a genetic study. J Med Genet 28: 443–447
31 Neumann HPH et al. (2002) Germ-line mutations in nonsyndromic pheochromocytoma. New Engl J Med 346: 1459–1466
32 Bryant J et al. (2003) Pheochromocytoma: the expanding genetic differential diagnosis. J Natl Cancer Inst 95: 1196–1204
33 Gagel RF et al. (1988) The clinical outcome of prospective screening for multiple endocrine neoplasia type 2a. An 18-year experience. N Engl J Med 318: 478–484
34 Mulligan LM et al. (1993) Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature 363: 458–460
35 Zeiger MA et al. (1995) Loss of heterozygosity on the short arm of chromosome 3 in sporadic, von Hippel-Lindau disease-associated, and familial pheochromocytoma. Genes Chromosomes Cancer 13: 151–156
36 Jimenez C et al. (2006) Should patients with apparently sporadic pheochromocytomas or paragangliomas be screened for hereditary syndromes? J Clin Endocrinol Metab 91: 2851–2858
37 Elder EE et al. (2005) Pheochromocytoma and functional paraganglioma syndrome: no longer the 10% tumor. J Surg Oncol 89: 193–201
38 Lenders JW et al. (2005) Phaeochromocytoma. Lancet 366: 665–675
39 Neumann HP et al. (2002) Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 346: 1459–1466
40 Amar L et al. (2005) Genetic testing in pheochromocytoma or functional paraganglioma. J Clin Oncol 23: 8812–8818
41 Benn DE et al. (2005) Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab 91: 790–792
42 Barontini M et al. (2006) Characteristics of pheochromocytoma in a 4- to 20-year-old population. Ann NY Acad Sci 1073: 30–37
43 Weinhausel A et al. (2003) Long-term follow up of a “sporadic” unilateral pheochromocytoma revealing multiple endocrine neoplasia MEN2A-2 in an elderly woman. Endocr Pathol 14: 375–382
NCPEM_2005_152.indd 101NCPEM_2005_152.indd 101 8/1/07 1:42:58 pm8/1/07 1:42:58 pm

REVIEW
102 NATURE CLINICAL PRACTICE ENDOCRINOLOGY & METABOLISM PACAK ET AL. FEBRUARY 2007 VOL 3 NO 2
www.nature.com/clinicalpractice/endmet
44 Astuti D et al. (2003) Genetic analysis of mitochondrial complex II subunits SDHD, SDHB and SDHC in paraganglioma and phaeochromocytoma susceptibility. Clin Endocrinol (Oxf) 59: 728–733
45 Eisenhofer G et al. (1999) Plasma normetanephrine and metanephrine for detecting pheochromocytoma in von Hippel-Lindau disease and multiple endocrine neoplasia type 2. N Engl J Med 340: 1872–1879
46 Bravo EL and Tagle R (2003) Pheochromocytoma: state-of-the-art and future prospects. Endocr Rev 24: 539–553
47 Kinney MA et al. (2002) Perioperative management of pheochromocytoma. J Cardiothorac Vasc Anesth 16: 359–369
48 Pacak K et al. (2001) Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med 134: 315–329
49 Prys-Roberts C (2000) Phaeochromocytoma—recent progress in its management. Br J Anaesth 85: 44–57
50 Proye C et al. (1989) Exclusive use of calcium channel blockers in preoperative and intraoperative control of pheochromocytomas: hemodynamics and free catecholamine assays in ten consecutive patients. Surgery 106: 1149–1154
51 Plouin PF et al. (1997) Tumor recurrence and hypertension persistence after successful pheochromocytoma operation. Hypertension 29: 1133–1139
52 Janetschek G et al. (1998) Laparoscopic surgery for pheochromocytoma: adrenalectomy, partial resection, excision of paragangliomas. J Urol 160: 330–334
53 Brunt LM et al. (2002) Adrenalectomy for familial pheochromocytoma in the laparoscopic era. Ann Surg 235: 713–720
54 Lee J et al. (1996) Cortical-sparing adrenalectomy for patients with bilateral pheochromocytoma. Surgery 120: 1064–1070
55 Nambirajan T et al. (2005) Laparoscopic adrenal surgery for recurrent tumours in patients with hereditary phaeochromocytoma. Eur Urol 47: 622–626
56 Yip L et al. (2004) Surgical management of hereditary pheochromocytoma. J Am Coll Surg 198: 525–534
57 Koch CA et al. (2002) Pheochromocytoma in von Hippel-Lindau disease: Distinct histopathologic phenotype compared to pheochromocytoma in multiple endocrine neoplasia type 2. Endocr Pathol 13: 17–27
58 DeLellis RA et al. (Eds; 2004) Tumours of Endocrine Organs. Lyon: IARC Press
59 Kimura N et al. (2005) Histological grading of adrenal and extra-adrenal pheochromocytomas and relationship to prognosis: a clinicopathological analysis of 116 adrenal pheochromocytomas and 30 extra-adrenal sympathetic paragangliomas including 38 malignant tumors. Endocr Pathol 16: 23–32
60 Linnoila RI et al. (1990) Histopathology of benign versus malignant sympathoadrenal paragangliomas: clinicopathologic study of 120 cases including unusual histologic features. Hum Pathol 21: 1168–1180
61 Thompson LD (2002) Pheochromocytoma of the Adrenal gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol 26: 551–566
62 Lack EE et al. (2003) Recommendations for the reporting of extra-adrenal paragangliomas. The Association of Directors of Anatomic and Surgical Pathology. Hum Pathol 34: 112–113
63 Association of Directors of Anatomic and Surgical Pathology [http://www.adasp.org] (accessed 15 September 2006)
64 Lack EE (1999) Recommendations for the reporting of tumors of the adrenal cortex and medulla. Association of Directors of Anatomic and Surgical Pathology. Virchows Arch 435: 87–91
65 The Royal College of Pathologists [http://www.rcpath.org] (accessed 15 September 2006)
66 Eisenhofer G et al. (2004) Malignant pheochromocytoma: current status and initiatives for future progress. Endocr Relat Cancer 11: 423–436
67 August C et al. (2004) CGH and CD 44/MIB-1 immunohistochemistry are helpful to distinguish metastasized from nonmetastasized sporadic pheochromocytomas. Mod Pathol 17: 1119–1128
68 Goldstein RE et al. (1999) Clinical experience over 48 years with pheochromocytoma. Ann Surg 229: 755–764
69 John H et al. (1999) Pheochromocytomas: can malignant potential be predicted? Urology 53: 679–683
70 Proye CA et al. (1994) “The” pheochromocytoma: a benign, intra-adrenal, hypertensive, sporadic unilateral tumor. Does it exist? World J Surg 18: 467–472
71 Whalen RK et al. (1992) Extra-adrenal pheochromocytoma. J Urol 147: 1–10
72 Mundschenk J and Lehnert H (1998) Malignant pheochromocytoma. Exp Clin Endocrinol Diabetes 106: 373–376
73 Brouwers FM et al. (2005) Low molecular weight proteomic information distinguishes metastatic from benign pheochromocytoma. Endocr Relat Cancer 12: 263–272
74 Averbuch SD et al. (1988) Malignant pheochromocytoma: effective treatment with a combination of cyclophosphamide, vincristine, and dacarbazine. Ann Intern Med 109: 267–273
75 Rose B et al. (2003) High-dose 131I-metaiodobenzylguanidine therapy for 12 patients with malignant pheochromocytoma. Cancer 98: 239–248
76 Safford SD et al. (2003) Iodine-131 metaiodobenzylguanidine is an effective treatment for malignant pheochromocytoma and paraganglioma. Surgery 134: 956–962
77 Takahashi K et al. (1999) Malignant pheochromocytoma with multiple hepatic metastases treated by chemotherapy and transcatheter arterial embolization. Intern Med 38: 349–354
78 Loh KC et al. (1997) The treatment of malignant pheochromocytoma with iodine-131 metaiodobenzylguanidine (131I-MIBG): a comprehensive review of 116 reported patients. J Endocrinol Invest 20: 648–658
79 Mukherjee JJ et al. (2001) Treatment of metastatic carcinoid tumours, phaeochromocytoma, paraganglioma and medullary carcinoma of the thyroid with (131)I-meta-iodobenzylguanidine [(131)I-mIBG]. Clin Endocrinol (Oxf) 55: 47–60
80 Chan EC and Ho PC (2000) High-performance liquid chromatography/atmospheric pressure chemical ionization mass spectrometric method for the analysis of catecholamines and metanephrines in human urine. Rapid Commun Mass Spectrom 14: 1959–1964
81 Crockett DK et al. (2002) Rapid analysis of metanephrine and normetanephrine in urine by gas chromatography-mass spectrometry. Clin Chem 48: 332–337
82 Lagerstedt SA et al. (2004) Measurement of plasma free metanephrine and normetanephrine by liquid chromatography-tandem mass spectrometry for diagnosis of pheochromocytoma. Clin Chem 50: 603–611
83 Taylor RL and Singh RJ (2002) Validation of liquid chromatography-tandem mass spectrometry method for analysis of urinary conjugated metanephrine and normetanephrine for screening of pheochromocytoma. Clin Chem 48: 533–539
Competing interestsThe authors declared they have no competing interests.
NCPEM_2005_152.indd 102NCPEM_2005_152.indd 102 8/1/07 1:42:59 pm8/1/07 1:42:59 pm






![Feocromocitoma [Modo de compatibilidad] · -Sd. Paragangliomas hereditarios. No se puede mostrar la imagen. Puede que su equipo no tenga suficiente memoria para abrir la imagen o](https://static.fdocuments.co/doc/165x107/5b89a85c7f8b9aa81a8ce6d3/feocromocitoma-modo-de-compatibilidad-sd-paragangliomas-hereditarios-no.jpg)